Acute Stress Disorder
Acute Stress Disorder (ASD) is a mental health problem that can occur in the first month after a traumatic event. The symptoms of ASD are like PTSD symptoms, but you must have them for longer than one month to have PTSD. Learn more about ASD and treatment options.
Reading time: minutes
How Common Is ASD?
Studies of ASD vary in terms of the tools used and the rates of ASD found. Overall, within one month of a trauma, survivors show rates of ASD ranging from 6% to 33%. Rates differ for different types of trauma. For example, survivors of accidents or disasters such as typhoons show lower rates of ASD. Survivors of violence such as robbery, assaults, and mass shootings show rates at the higher end of that range.
Who Is at Risk for ASD as a Result of Trauma?
Several factors can place you at higher risk for developing ASD after a trauma:
- Having gone through other traumatic events
- Having had PTSD in the past
- Having had prior mental health problems
- Tending to have symptoms, such as not knowing who or where you are, when confronted with trauma
Does ASD Predict PTSD?
If you have ASD, you are very likely to get PTSD. Research has found that over 80% of people with ASD have PTSD six months later. Not everyone with ASD will get PTSD, though.
Also, those who do not get ASD can still develop PTSD later on. Studies indicate that a small number (4% to 13%) of survivors who do not get ASD in the first month after a trauma will get PTSD in later months or years.
Are There Effective Treatments for ASD?
Yes, a type of treatment called cognitive behavioral therapy (CBT) has been shown to have positive results. Research shows that survivors who get CBT soon after going through a trauma are less likely to get PTSD symptoms later. A mental health care provider trained in treatment for trauma can judge whether CBT may be useful for a trauma survivor.
Another treatment called psychological debriefing (PD) has sometimes been used in the wake of a traumatic event. However, there is little research to back its use for effectively treating ASD or PTSD. It should also be noted that with more severe trauma or reactions such as PTSD, debriefing is not recommended.
Our bodies and minds are ready to mobilize at times of stress and danger in case we need to protect our lives or others’. Our heart rate, blood pressure, breathing, and metabolism will increase, and we’ll tense up, ready to fight or to flee from the danger. This physiological preparation might save our lives, but for some people, this activation is a one-way ticket and their bodies may not be as prepared to handle the aftermath. In fact, this stress response may not return to its dormant state but continue to fire up at times when someone is reminded of that original traumatic event—even if they aren’t actually in danger. It can creep up and feel out of control, significantly affecting one’s regular life functioning, relationships, and connection to life. In this case of a persistent stress response, not only has the person not been able to process their experience and feelings around the original trauma, but they are also frequently suffering through this heightened fight-or-flight reaction. This disordered experience can be very distressing.
It makes sense that we would endure significant distress after a traumatic event—be it a natural disaster, a violent assault, a car accident, or even just hearing in detail about the anguish someone else has experienced. But as this distress lasts beyond a couple of days, it can be classified as a disorder in need of therapeutic attention. Comparing acute stress disorder vs. post-traumatic stress disorder has to do with how long the distressing symptoms last following the event or how much time passes between the event and the onset of symptoms. With either disorder, the best chances for recovery are with early and comprehensive treatment, so an individual can finally process their pain and stress and develop coping strategies in the face of future stressors and triggers.
Posttraumatic stress disorder (PTSD) is a psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event, series of events or set of circumstances. An individual may experience this as emotionally or physically harmful or life-threatening and may affect mental, physical, social, and/or spiritual well-being. Examples include natural disasters, serious accidents, terrorist acts, war/combat, rape/sexual assault, historical trauma, intimate partner violence and bullying,
PTSD has been known by many names in the past, such as “shell shock” during the years of World War I and “combat fatigue” after World War II, but PTSD does not just happen to combat veterans. PTSD can occur in all people, of any ethnicity, nationality or culture, and at any age. PTSD affects approximately 3.5 percent of U.S. adults every year. The lifetime prevalence of PTSD in adolescents ages 13 -18 is 8%. An estimate one in 11 people will be diagnosed with PTSD in their lifetime. Women are twice as likely as men to have PTSD. Three ethnic groups – U.S. Latinos, African Americans, and Native Americans/Alaska Natives – are disproportionately affected and have higher rates of PTSD than non-Latino whites.
People with PTSD have intense, disturbing thoughts and feelings related to their experience that last long after the traumatic event has ended. They may relive the event through flashbacks or nightmares; they may feel sadness, fear or anger; and they may feel detached or estranged from other people. People with PTSD may avoid situations or people that remind them of the traumatic event, and they may have strong negative reactions to something as ordinary as a loud noise or an accidental touch.
A diagnosis of PTSD requires exposure to an upsetting traumatic event. Exposure includes directly experiencing an event, witnessing a traumatic event happening to others, or learning that a traumatic event happened to a close family member or friend. It can also occur as a result of repeated exposure to horrible details of trauma such as police officers exposed to details of child abuse cases.
Symptoms and Diagnosis
Symptoms of PTSD fall into the following four categories. Specific symptoms can vary in severity.
- Intrusion: Intrusive thoughts such as repeated, involuntary memories; distressing dreams; or flashbacks of the traumatic event. Flashbacks may be so vivid that people feel they are reliving the traumatic experience or seeing it before their eyes.
- Avoidance: Avoiding reminders of the traumatic event may include avoiding people, places, activities, objects and situations that may trigger distressing memories. People may try to avoid remembering or thinking about the traumatic event. They may resist talking about what happened or how they feel about it.
- Alterations in cognition and mood: Inability to remember important aspects of the traumatic event, negative thoughts and feelings leading to ongoing and distorted beliefs about oneself or others (e.g., “I am bad,” “No one can be trusted”); distorted thoughts about the cause or consequences of the event leading to wrongly blaming self or other; ongoing fear, horror, anger, guilt or shame; much less interest in activities previously enjoyed; feeling detached or estranged from others; or being unable to experience positive emotions (a void of happiness or satisfaction).
- Alterations in arousal and reactivity: Arousal and reactive symptoms may include being irritable and having angry outbursts; behaving recklessly or in a self-destructive way; being overly watchful of one’s surroundings in a suspecting way; being easily startled; or having problems concentrating or sleeping.
Many people who are exposed to a traumatic event experience symptoms similar to those described above in the days following the event. For a person to be diagnosed with PTSD, however, symptoms must last for more than a month and must cause significant distress or problems in the individual’s daily functioning. Many individuals develop symptoms within three months of the trauma, but symptoms may appear later and often persist for months and sometimes years. PTSD often occurs with other related conditions, such as depression, substance use, memory problems and other physical and mental health problems.
Related Conditions
Acute Stress Disorder
Acute stress disorder occurs in reaction to a traumatic event, just as PTSD does, and the symptoms are similar. However, the symptoms occur between three days and one month after the event. People with acute stress disorder may relive the trauma, have flashbacks or nightmares and may feel numb or detached from themselves. These symptoms cause major distress and problems in their daily lives. About half of people with acute stress disorder go on to have PTSD. Acute stress disorder has been diagnosed in 19%-50% of individuals that experience interpersonal violence (e.g., rape, assault, intimate partner violence).
Psychotherapy, including cognitive behavior therapy can help control symptoms and help prevent them from getting worse and developing into PTSD. Medication, such as SSRI antidepressants can help ease the symptoms.
Adjustment Disorder
Adjustment disorder occurs in response to a stressful life event (or events). The emotional or behavioral symptoms a person experiences in response to the stressor are generally more severe or more intense than what would be reasonably expected for the type of event that occurred.
Symptoms can include feeling tense, sad or hopeless; withdrawing from other people; acting defiantly or showing impulsive behavior; or physical manifestations like tremors, palpitations, and headaches. The symptoms cause significant distress or problems functioning in key areas of someone’s life, for example, at work, school or in social interactions. Symptoms of adjustment disorders begin within three months of a stressful event and last no longer than six months after the stressor or its consequences have ended.
The stressor may be a single event (such as a romantic breakup), or there may be more than one event with a cumulative effect. Stressors may be recurring or continuous (such as an ongoing painful illness with increasing disability). Stressors may affect a single individual, an entire family, or a larger group or community (for example, in the case of a natural disaster).
An estimated 5% to 20% of individuals in outpatient mental health treatment have a principal diagnosis of adjustment disorder. A recent study found that more than 15% of adults with cancer had adjustment disorder. It is typically treated with psychotherapy.
Disinhibited Social Engagement Disorder
Disinhibited social engagement disorder occurs in children who have experienced severe social neglect or deprivation before the age of two. Similar to reactive attachment disorder, it can occur when children lack the basic emotional needs for comfort, stimulation and affection, or when repeated changes in caregivers (such as frequent foster care changes) prevent them from forming stable attachments.
Disinhibited social engagement disorder involves a child engaging in overly familiar or culturally inappropriate behavior with unfamiliar adults. For example, the child may be willing to go off with an unfamiliar adult with minimal or no hesitation. Developmental delays including cognitive and language delays often co-occur with this disorder. Caregiving quality has been shown to mediate the course of this illness. Yet even with improvements in the caregiving environment some children may have symptoms that persist through adolescence.
The prevalence of disinhibited social engagement disorder is unknown, but it is thought to be rare. Most severely neglected children do not develop the disorder. The most important treatment modality is to work with caregivers to ensure the child has an emotionally available attachment figure.
Reactive Attachment Disorder
Reactive attachment disorder occurs in children who have experienced severe social neglect or deprivation during their first years of life. It can occur when children lack the basic emotional needs for comfort, stimulation and affection, or when repeated changes in caregivers (such as frequent foster care changes) prevent them from forming stable attachments.
Children with reactive attachment disorder are emotionally withdrawn from their adult caregivers. They rarely turn to caregivers for comfort, support or protection or do not respond to comforting when they are distressed. During routine interactions with caregivers, they show little positive emotion and may show unexplained fear or sadness. The problems appear before age 5. Developmental delays, especially cognitive and language delays, often occur along with the disorder.
Reactive attachment disorder is uncommon, even in severely neglected children. Treatment involves a therapist working with a child and their family in order to strengthen the relationship between the child and their primary caregivers.
Treatment
It is important to note that not everyone who experiences trauma develops PTSD, and not everyone who develops PTSD requires psychiatric treatment. For some people, symptoms of PTSD subside or disappear over time. Others get better with the help of their support system (family, friends or clergy). But many people with PTSD need professional treatment to recover from psychological distress that can be intense and disabling. It is important to remember that trauma may lead to severe distress. That distress is not the individual’s fault, and PTSD is treatable. The earlier a person gets treatment, the better chance of recovery.
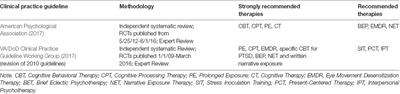
Psychiatrists and other mental health professionals use various effective (research-proven) methods to help people recover from PTSD. Both talk therapy (psychotherapy) and medication provide effective evidence-based treatments for PTSD.
Cognitive Behavioral Therapy
One category of psychotherapy, cognitive behavior therapies (CBT), is very effective. Cognitive processing therapy, prolonged exposure therapy and stress inoculation therapy (described below) are among the types of CBT used to treat PTSD.
- Cognitive Processing Therapy is an evidence-based, cognitive behavioral therapy designed specifically to treat PTSD and comorbid symptoms. It focuses on changing painful negative emotions (such as shame, guilt, etc.) and beliefs (such as “I have failed;” “the world is dangerous”) due to the trauma. Therapists help the person confront such distressing memories and emotions.
- Prolonged Exposure Therapy uses repeated, detailed imagining of the trauma or progressive exposures to symptom “triggers” in a safe, controlled way to help a person face and gain control of fear and distress and learn to cope. For example, virtual reality programs have been used to help war veterans with PTSD re-experience the battlefield in a controlled, therapeutic way.
- Trauma Focused Cognitive Behavioral Therapy is an evidence-based treatment model for children and adolescents that incorporates trauma-sensitive interventions with cognitive behavioral, family, and humanistic principles and techniques.
- Eye Movement Desensitization and Reprocessing for PTSD is a trauma-focused psychotherapy which is administered over approximately 3 months. This therapy helps a person to reprocess the memory of the trauma so that it is experienced in a different way. After a thorough history is taken and a treatment plan developed the therapist guides the patient through questions about the traumatic memory. Eye movements similar to those in REM sleep is recreated during a session by having the patient watch the therapist’s fingers go back and forth or by watching a light bar. The eye movements last for a brief time period and then stop. Experiences during a session may include changes in thoughts, images, and feelings. After repeated sessions the memory tends to change and is experienced in a less negative manner.
- Group therapy encourages survivors of similar traumatic events to share their experiences and reactions in a comfortable and non-judgmental setting. Group members help one another realize that many people would have responded the same way and felt the same emotions. Family therapy may also help because the behavior and distress of the person with PTSD can affect the entire family.
Other psychotherapies such as interpersonal, supportive and psychodynamic therapies focus on the emotional and interpersonal aspects of PTSD. These may be helpful for people who do not want to expose themselves to reminders of their traumas.
Medication
Medication can help to control the symptoms of PTSD. In addition, the symptom relief that medication provides allows many people to participate more effectively in psychotherapy.
Some antidepressants such as SSRIs and SNRIs (selective serotonin re-uptake inhibitors and serotonin-norepinephrine re-uptake inhibitors), are commonly used to treat the core symptoms of PTSD. They are used either alone or in combination with psychotherapy or other treatments.
Other medications may be used to lower anxiety and physical agitation, or treat the nightmares and sleep problems that trouble many people with PTSD.
Other Treatments
Other treatments including complementary and alternative therapies are also increasingly being used to help people with PTSD. These approaches provide treatment outside the conventional mental health clinic and may require less talking and disclosure than psychotherapy. Examples include acupuncture, yoga and animal-assisted therapy.
In addition to treatment, many people with PTSD find it very helpful to share their experiences and feelings with others who have similar experiences, such as in a peer support group.
References
- American Psychiatric Association. (2022). Trauma- and Stressor-Related Disorders. In Diagnostic and Statistical Manual of Mental Disorders (5th ed., text rev.).
- Bichitra Nanda Patra and Siddharth Sarkar. Adjustment Disorder: Current Diagnostic Status. Indian J Psychol Med. 2013 Jan-Mar; 35(1): 4–9.
- Harvard Medical School. (2007). National Comorbidity Survey (NCS). (2017, August 21). Data Table 2: 12-month prevalence DSM-IV/WMH-CIDI disorders by sex and cohort.
- National Library of Medicine: MedlinePlus. Adjustment Disorder.
- American Academy of Child and Adolescent Psychiatry. Facts for Families: Attachment Disorders.
- Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.>
- Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. HHS Publication No. (SMA) 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.
Physician Review
Monica Taylor-Desir, M.D., M.P.H., DFAPA
November 2022