Many biological predispositions exist for anxiety and depression. Mood and anxiety disorders are among the most common types of mental disorders. These conditions are debilitating and are associated with considerable costs at an economic, societal, and personal level.
Common treatment options for such disorders include pharmacotherapy and psychotherapy. But new research shows that medications for anxiety, depression, and related symptoms such as insomnia are only slightly more effective than placebo treatments. Additionally, not all patients respond positively to pharmacotherapy or psychotherapy and often experience unpleasant side effects.
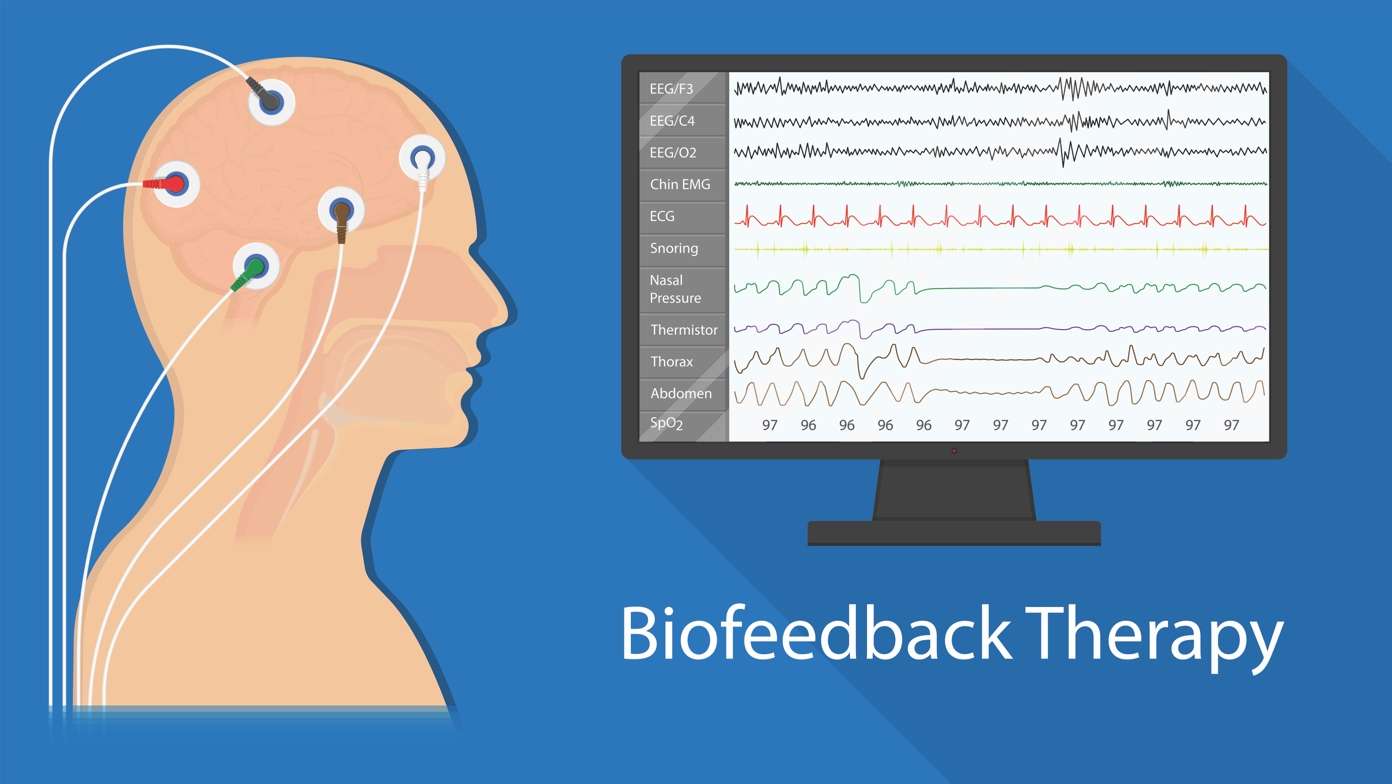
The good news is there are other treatment options that can be quite effective, such as biofeedback. Biofeedback is a non-invasive treatment technique that helps patients get feedback from how their body or brain is functioning and then use that information to improve their body or brain function. In biofeedback therapy, a person’s psychophysiological state is captured by specials sensors that measure heart rate, respiration, blood pressure, or brain activity. With the patient receives this information, he/she can then try to change his/her heart rate, breathing rate, blood pressure, or brain activity.
For example, a biofeedback device can show that your heart rate races at 100; then you can take deep breaths for 10-15 minutes, and your heart rate gradually falls to 80-90. If you do this exercise twice a day for two months, your baseline heart rate becomes calmer – even when you are not trying to focus on breathing slowly. Such treatment can over time improve your blood pressure and reduce your risk for heart attacks and strokes.

Neurofeedback Therapy
A specific type of biofeedback is neurofeedback therapy or Neurotherapy. Neurofeedback is a research-based intervention that can improve your brain function through brain training exercises.

Your brain cells can become overactive when you are anxious or stressed out. But your brain can “learn” to calm down if you were to receive input about how overactive your brain is (just as you can appreciate how fast your heart is racing if you were to have a device that measures your pulse). The electrical activity of your brain (known as “brain waves”) can be measured by sensors placed on your head (similar to EKG sensors that are used to measure heart activity). Neurofeedback trains a patient’s brain to improve the brainwave patterns by way of computer technology. The feedback is administered to the patient in real-time, by using video images or by using sounds. Neurofeedback can lead to behavioral changes for relaxation and better mood.
Brain science has proven that repetitive exercise of brain networks, such as that involved with neurofeedback, has the ability to reshape the brain. It helps to optimize brain wave patterns while enhancing connections between neurons and networks. Neurofeedback therapy also improves the parasympathetic nervous system while slowing blood pressure and heart rate. After 20-60 sessions of neurofeedback, many patients experience a reduction of their anxiety and depression symptoms.
Neurofeedback for Depression and Anxiety
A great deal of scientific evidence in the past 30 years has provided evidence for the effectiveness of neurofeedback as a treatment modality for anxiety and depression. In each study, anxiety and/or depression were reduced after neurofeedback training was administered for three months.
One method for reducing anxiety with neurofeedback has been shown in a publication in Psychotherapy and Psychosomatics. Deficient emotion regulation can be a marker for anxiety. These deficits are closely linked to impaired prefrontal regulatory control (the “logical parts of the brain) over the amygdala, a part of the brain that is tightly linked with emotions such as anxiety. Thankfully this impairment is sensitive to treatment with neurofeedback which leads to a reduction in symptoms of anxiety.
Numerous studies have shown that a person’s mood is positive when the left frontal area of the brain is more active than the right frontal region – and that the mood is poor when the right is more active than the left. Neurofeedback therapy uses this established finding to treat depression. According to multiple controlled studies, the mood was improved when the left front side of the brain was trained to be more active than the right by way of neurofeedback therapy.
A study by Dr. Majid Fotuhi and his colleagues showed that neurofeedback therapy, especially when combined with another form of biofeedback that involved breathing slowly (called Heart Rate Variability training) can be quite effective for reducing symptoms of both anxiety and depression. They performed an assessment with the Achenbach System of Empirically Based Assessment (ASEBA) symptom checklist. 183 of the 334 clients had abnormal scores for depression, anxiety, or both. During the study, clients experienced substantial improvement after 30 sessions of neurofeedback and heart rate variability training. More importantly, many of the clients fell into the normal group after treatment. And for clients who exemplified the most severe symptoms of anxiety and depression, 57.1% of those with severe anxiety and 45.8% of those with severe depression fell into the normal group after treatment.
Evidence from many other studies in recent years continues to show that neurofeedback is a viable treatment option for patients who suffer from anxiety, depression, and related symptoms such as poor sleep, difficulty with attention, and brain fog. Click here for more information on neurofeedback services at NeuroGrow.
This blog is written by Mrs. Courtney Cosby and edited by Dr. Majid Fotuhi.
Two years ago, I walked through the door of a Seattle therapist’s office with the goal of resetting my 45-year-old brain. A trauma survivor with a history of depression and anxiety, I was hoping that an alternative mode of therapy I’d heard about called neurofeedback might finally alleviate my more stubborn symptoms.
At the time, the simple act of swerving my car to avoid a pothole or tripping over my dog triggered my body’s fight-or-flight response—vestiges of a childhood spent with a psychotic mother. I had other issues, too: inadequate concentration, difficulty with decision-making, and a strangely selective memory. I never forgot numbers, whether my seventh-grade boyfriend’s birthday or the six-digit codes of items I rang up as a cashier during college, but words proved trickier. Any meaningful vocabulary growth peaked at about age 15. For a writer, this is problematic.
Advertisement
Having given a fair shot to the more popular treatments, I was driven to seek one less common.
Neurofeedback wasn’t my first attempt at improving my mental health. I’d tried, or still used, psychotherapy, antidepressants, homeopathy, hypnotherapy, diet modifications, exercise, meditation, and acupuncture. Some modalities had a greater impact than others, and all of them helped me to some degree. But even when I was able to keep the worst symptoms in check, other lurking issues detracted from my sense of “being okay.” Having given a fair shot to the more popular treatments, I was driven to seek one less common.
Neurofeedback, also known as EEG biofeedback or brain biofeedback, fit the bill. During a typical treatment, sensors are placed on the head to capture the frequency and power of the brain’s electrical activity, visually represented by the five types of brain waves: delta, theta, alpha, beta, and gamma. Very generally, neurofeedback is a process by which therapists attempt to regulate brain waves. They do this by tracking your brain activity on a computer and then repeatedly send this information back to the brain via computer imagery or an electrical signal. Because there are still a lot of questions about how exactly the treatment works—assuming it does work—the details can vary depending on the therapist, however. As the Washington Post explains:
A patient might watch a movie, for example, while hooked to sensors that send data to a computer. A therapist, following the brain activity on a monitor, programs the computer to stop the movie if an abnormal number of fast or slow brain waves is detected or if the brain waves are erratic, moving rapidly from fast to slow waves.
Advertisement
According to the Washington Post, in addition to depression and anxiety, neurofeedback is currently being used to treat a number of other conditions including attention deficit disorder, attention deficit/hyperactivity disorder, addiction, autism spectrum disorder, chronic fatigue, learning disabilities, obsessive-compulsive disorder, post-traumatic stress disorder, tics and seizures, and traumatic brain injuries. This wide application spectrum is part of the reason I was drawn to the treatment. I wondered if some of my brain’s problematic tendencies might be attributed to conditions beyond depression and anxiety. Could neurofeedback be a complete 60,000-mile service for the price of an oil change?
Anyone who has suffered from mental illness knows how important hope is during the search for solutions.
To be clear, I made a deliberate choice to be hopeful about neurofeedback’s possibilities. I think anyone who has ever suffered from a mental illness knows how important hope is during the often long and frustrating search for solutions. People’s responses to the “tried-and-tested” treatments vary. It’s not unusual for those treatments to fail, or at least, to not fully succeed. Even after 60-plus years of ever-increasing use, antidepressants and their efficacy remain a debated topic. Indeed, researchers continue to attempt to answer the most basic questions, like why people get depression. Brain science remains so fluid that I’m surprised no one has written a book called “Fifty Shades of Grey Matter” yet.
Those who question neurofeedback’s potency point to a lack of conclusive evidence that its effects are permanent, or even long lasting, after treatment has ceased. This is a fair critique and much more research needs to be done in order to figure out what exactly neurofeedback is accomplishing. But my experiences with psychotropic medication have shown similar problems. I started on paroxetine (the Paxil generic) in my 20s. It abruptly stopped working in my 30s—while I was taking it—and I slogged through five other medication trials before I found an effective replacement. Since then, paroxetine has been identified as having anti-cholinergic effects, which can include cognitive impairment and memory loss.
Advertisement
Those who question neurofeedback’s potency point to a lack of conclusive evidence.
At the same time, the pharmacological revolution has stifled interest in electrophysiology for decades, as Dr. Bessel van der Kolk notes in his 2014 book The Body Keeps The Score. An additional challenge lies in the lack of available grant money for studies. Dr. Mary Lee Esty, who has researched and practiced neurofeedback in Maryland for 25 years, told Quartz that she’s had to self-fund several research projects. As she put it, “How else was it going to get done?”
Today, neurofeedback research is on the upswing. Most studies to date have examined its use in treating ADHD in children. Other studies heralded as promising by neurofeedback advocates have failed to convince skeptics either because they weren’t large enough or because they weren’t a double-blind, randomized controlled trial—the so-called “gold standard” for new treatments. However, outcomes are solid enough that in 2012, the American Academy of Pediatrics approved biofeedback as a Level 1 “best support” treatment option for children with ADHD.
Neurofeedback as treatment for PTSD in military vets is also being studied. Data collected in 2011 by “Homecoming for Veterans,” a no-cost neurofeedback initiative of California’s The EEG Institute, has proved positive. In 2015, Esty and her research partner Dr. David V. Nelson published outcomes of two different studies in the journals Military Medical Research and Military Medicine respectively. Though the sample sizes were quite small, again due to funding constraints, the findings reported a significant reduction in symptoms for all but one study participant.
Advertisement
As neurofeedback graduates from what Esty calls its “late adolescence,” she feels it’s finding a wider audience in the brain-health field. She cites her invitation to present at the Nevada Psychiatric Association’s 22nd National Psychopharmacology Update in February 2017, as an example.
As neurofeedback graduates from its “late adolescence,” it’s finding a wider audience in the brain-health field.
As for my own experience, I continued treatment once a week for three months—with a six-week break in the middle—before tapering to every two weeks for another two months. The therapist shared data with me at intervals, first collecting a baseline of the 21 sites on my brain and then tailoring my treatment based on what we saw.
More than half of the sites lacked any measurable electrical activity. The therapist called this “suppression,” a common pattern for a trauma survivor. If a brain is triggered enough times for protection and survival, and the stress hormone cortisol is released, cell and neuron development are altered, and an excess of myelin, or white matter, develops. Communication slows between the amygdala (responsible for emotional processing) and the prefontal cortex (responsible for memory, learning, decision-making, and the like), while it increases between the amygdala and the hypothalamus, where fight-or-flight begins.
Advertisement
I had the unfamiliar sense that all the parts of my brain were at the party—and not a frat-house fiesta, either.
When the therapist focused my treatment on reengaging the suppressed sites, electrical activity returned—score a win for neuroplasticity. I stopped treatment once the improvement in my sense of well-being seemed to plateau. But I felt clearer: instead of stumbling, I could glide through my days.
This shift took up full-time residence somewhere around my eighth session. I had the unfamiliar sense that all the parts of my brain were at the party—and not a frat-house fiesta, either. This translated into a respite from the normal cognitive grind as my decision-making struggles abated and I experienced days of intense (for me) productivity. I felt more certain about my actions in general—the analysis paralysis and second-guessing that had always been a big part of my “technique” quieted.
What didn’t change was my hair-trigger fight-or-flight response, nor did my memory or learning retention improve. That was disheartening, but only for a moment. Rather than attribute the unresponsiveness to a neurofeedback failure, I view it as further confirmation of the brain’s complicated circuitry.
Advertisement
In terms of longevity, my very anecdotal assessment has been that most of the gains I made have stuck around, albeit not as pronounced. I still have occasional days of frustrating fog and lack of clarity. But none of these setbacks have derailed me from my overall quest for mental health solutions. Doing layperson research is part of being my own best mental health advocate, and I’m keeping my ear to the ground.