At the Johns Hopkins Department of Physical Medicine and Rehabilitation, our occupational therapists specialize in helping patients with mental health disorders. Our occupational therapists are experts in performing behavioral health assessments, which offer insight into a patient’s condition. They have strong observation and creative problem-solving skills, and understand human development and function across different diagnoses.
Why Choose Johns Hopkins

Patients may have challenges in the areas of planning tasks, organizing, problem solving and decision making. They may also have difficulties with controlling emotions, which can make it difficult to function and be independent in society. Occupational therapy can help improve on or compensate for these challenges. Our occupational therapists use standardized and nonstandardized screening and assessments to make recommendations for treatment, which may include:
- Patient and caregiver education
- Practicing life management skills
- Adapting tasks or environment to become more independent
- Developing coping mechanisms to deal with emotional problems
Psychiatric Occupational Therapy Team
Our psychiatric occupational therapy team works closely with patients with mental illness. Our therapists help these patients improve their function in work, play, leisure, social life, self-care and community living skills. Our team is highly trained in assessing these skills and making recommendations for treatment and safe discharge.
-
Bobby Walsh, DBH, OTR/L, BCMH | Team Lead
AOTA Board Certification in Mental Health

-
Tess Spence, MS, OTR/L | Clinical Specialist

Helping Patients Enjoy Life to the Fullest
Our occupational therapists are trained to identify difficulties in performing daily activities. They help address these underlying problems through the activities listed above. Our team can work with patients and their loved ones to improve these and other life management skills:
- Creating and following a productive daily schedule
- Taking care of personal hygiene
- Managing one’s own health
- Navigating the community and using public transportation
- Organizing and following a medication regimen
- Interacting appropriately in work or social situations
- Working or volunteering
- Planning and cooking healthy meals
- Managing budget and finances
Developing Habits That Are Important to You

Habit training was the first occupational therapy treatment model. It was introduced by Eleanor Clarke Slagle, with input from psychiatrist Adolf Meyer, when both worked at Johns Hopkins in the early 1900s. Habit training focuses on balancing activities in the areas of work, rest and play, which can be unbalanced in people with mental health disorders. When occupational therapy was fairly new, habit training was heavily focused on arts and crafts. Now, our updated approach emphasizes meaningful activities rooted in independent living and quality of life.
Request an appointment with one of our mental health occupational therapy experts to discuss how we can help you or your loved one.
Locations and Referrals
Our psychiatric occupational therapy team is based in The Johns Hopkins Hospital and offers both inpatient and outpatient services, as well as partial hospitalization. Contact us if you are looking to make an appointment or refer a patient.
There are a lot of people who don’t know what occupational therapy is, but even fewer know about the role of OT in mental health. But in fact, the profession of occupational therapy first came to be known within psychiatric hospitals.
This is why the term occupational therapy contains the word occupation. Therapists who worked in behavioral health in the 1950s and 1960s would engage patients in meaningful occupations (or activities) in an attempt to keep them productive, attentive, and generally healthy. Handiwork was thought to have a large impact on the recovery process. The general idea behind this science is helpful, since individuals are often more motivated for rehabilitation if they can stay busy and feel useful.
Of course, the way they went about this is now viewed as overly simplistic and outdated, since the extent of their treatment would be working to complete arts and crafts such as basket weaving, lacing, and coloring.
The context of an OT’s role in mental health is the reason why we now delineate between activities and occupations. The purpose of OT is not simply to give our patients something to do, but rather to tailor treatment to the patient’s preferences, goals, and needs across a range of areas.
For this reason, mental health is thought of as one of the most customizable practice areas. Therapists in these settings are not typically held to the strict productivity standards that therapists in skilled nursing facilities and hospitals are. This means that an occupational therapist can use a high amount of creativity, planning time, and evaluation to understand what their patients need and work to make it happen.
The Role of OT in Mental Health
The role of a mental health occupational therapist varies slightly across inpatient and outpatient settings. But the goals are often shared in that treatment focuses on increasing a patient’s awareness of their condition (also called insight) and expanding the range of skills and tools they regularly use to manage their disorder.
One of the main ways that occupational therapists assist patients in behavioral health settings is through psychoeducational groups. These groups focus largely on education but as it directly pertains to someone’s condition. So rather than a standard educational group that involves telling someone what options they have in a certain area, psychoeducational groups show patients how they can engage in these areas despite symptoms, treatment plans, and more.

Psychoeducational groups in both outpatient and inpatient settings typically address the following topics:
Self-care
Self-care includes dressing, eating, toileting, bathing, and grooming. Therapists in nursing facilities may practice these skills in a hands-on way with patients. Therapists in mental health settings focus more on the barriers to self-care such as poor motivation, low energy, variable mood, unstable housing, and a lack of financial resources.
Relaxation and stress reduction techniques
Stress reduction techniques can range from hobby engagement, yoga, exercise, and many more strategies to engage in relaxation and therefore reduce levels of stress.
Coping strategies
This can differ from stress reduction in that coping skills can often be used in more subtle ways such as on public transportation, in the store, or at work. People can use techniques like deep breathing, brief periods of meditation, or guided imagery to cope with stress in the moment and improve their ability to function within the community.
Emotion regulation
Ranging from anger management to interpersonal dynamics to conflict resolution, this area is a great way to address uncomfortable feelings that are present with nearly every mental health concern. It is a good idea to focus on emotions that are especially uncomfortable such as abandonment, loneliness, fear of rejection, and unworthiness.
This may also include anger management, conflict resolution, interpersonal dynamics, social skills training, and more.
Symptom management
Education regarding symptom management often includes coping skills, stress reduction techniques, and emotion regulation. But a group solely focused on this topic should include personalized plans to deal with each patient’s symptoms. This makes it more powerful and far more effective for each person.
Instrumental activities of daily living (IADLs)
IADLs cover a wide range of topics intended to focus on those higher level self-care tasks such as health maintenance (including the management of medications, appointments, and other treatment-related requirements), budgeting, and household management such as laundry, driving, and cooking. These groups can be approached much the same as those focused on self-care in that education should crucially cover the factors that impact IADL completion.
Depending on the facility’s rules, funding, and physical treatment space, it may be appropriate or necessary to practice some of these skills in an individual or group atmosphere to assess a patient’s safety, function, and general capabilities in each area.
Community mobility or re-entry
Depending on the setting (inpatient or outpatient), education may cover accessing the community safely and effectively or reentering the community after a hospitalization. Some patients may benefit from instruction on using public transportation or ride shares, maps, medical transportation companies for appointments, online navigation systems, identifying signage, locating important buildings in their community such as the hospital, store, and police station.
Reentry groups can focus on social etiquette when in public settings, personal safety when around others, and some basic community navigation.
Social skills and communication
Along with emotion regulation, social skills are crucial to managing a mental health condition. Depending on the severity of someone’s condition and their level of functioning, some patients will benefit from education on acceptable social behavior such as how to utilize verbal and non-verbal cues, being sensitive around certain topics, giving respectful replies, disclosing an appropriate amount of information, and more.

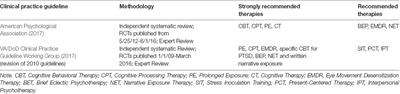
Diagnosis education
Far too often, patients don’t receive enough information about their own diagnoses or treatment plan. Education on what to expect with each condition is very helpful, including prognosis, treatment options (as provided by the patient’s doctor), medications, and adjunctive treatments.
It is important to note that, while you can talk about general symptoms that are common with many mental health concerns, it breaks HIPAA to discuss a person’s specific diagnosis or circumstances in a group setting. So if this type of education is indicated or requested by the patient, it is best to provide it during one-on-one time.
Individual roles
Each person has roles to fulfill and mental health concerns can often get in the way of that. It’s possible to complete a psychoeducational group that covers a range of roles in a general sense so that each person can get back to meaningful roles they prioritize. This may include being a daughter or son, grandparent, parent, worker, church member, volunteer, or caregiver. Either way, they should receive education on how to manage their condition while still engaging in these roles in the ways they wish to.
Productive leisure
Hobbies and leisure activity are another important area that can assist with recovery. Individuals may not be aware of viable leisure pursuits or they may have trouble participating due to motivation and other factors discussed earlier. For this reason, education should focus on helping patients successfully engage in whatever leisure activities are of interest to them.
_______________
The above areas serve as the crux of occupational therapy treatment in both community-based settings such as outpatient clinics, clubhouses, and drop-in centers, as well as inpatient settings such as hospitals and residential facilities. Occupational therapists have a large impact on the rehabilitation process of individuals living with any type of mental health concern.
This is yet another meaningful way that OTs can impact change and assist the movement toward improving our society’s mental health.
What is your favorite way that OTs can address mental health? What would you add about the role of OT in mental health in general? Let us know in the comments!
And for more about mental health occupational therapy, be sure to check out our other article, Occupational Therapy in Mental Health: An Overview of 6 Typical Settings.