Summary
Cell biologist Michael Overholtzer explains apoptosis, a form of programmed cell death that can lead to cancer when it doesn’t function properly.
The death of one tiny cell might seem like a simple thing. But the process is much more complicated than you would expect.
There are actually several types of cell death, each with its own unique characteristics and processes. One of the most well-studied is called apoptosis.
“Apoptosis is defined by a set of physical, often visible, features that are associated with the demise of an individual cell,” says Memorial Sloan Kettering cell biologist Michael Overholtzer. “It’s probably one of the most common forms of cell death during the development of an organism. It also plays an important role in cancer.”
One purpose of apoptosis is to eliminate cells that contain potentially dangerous mutations. If a cell’s apoptosis function is not working properly, the cell can grow and divide uncontrollably and ultimately create a tumor.
Visible Changes, Molecular Changes
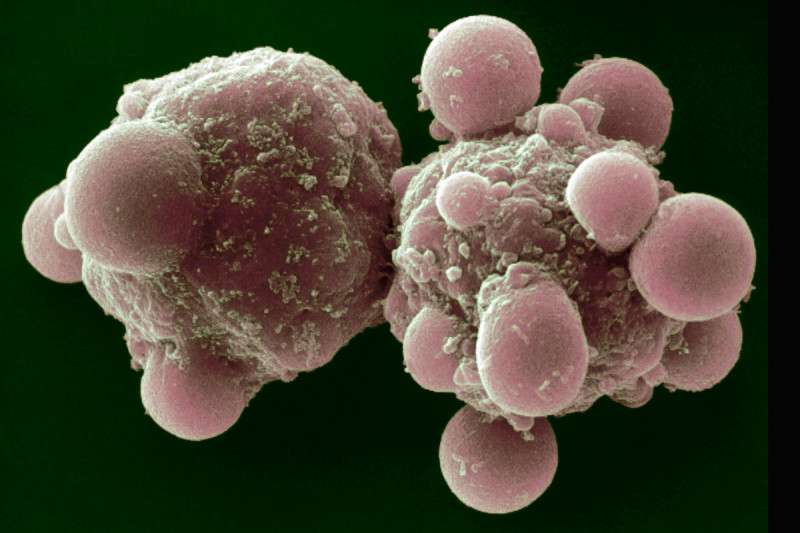
So what do you see if you look at an apoptotic cell under a microscope? “The nucleus looks shrunken or condensed and fragmented into pieces, whereas a normal nucleus is one round oval,” Dr. Overholtzer explains.
“The other obvious feature is that the cells themselves would shrink and begin to bleb,” he adds. “Blebbing means that the cell’s membrane changes, and there are bulging protrusions from the surface of the cell.”
An enzyme called caspase starts the chain reaction of changes that lead to a cell’s death by apoptosis. “Caspase is essentially like molecular scissors,” Dr. Overholtzer says. “In a normal, happy cell, it’s inactive, but once a cell is either put under stress or developmentally programmed to commit suicide, the scissors are activated and start to cut up certain proteins inside the cell, beginning the apoptosis process.”
In cancer cells, however, the scissors may not get the signal to start cutting. “The sensor that recognizes cell damage may not work, and the signal is never sent,” he says. “There are currently strategies under way to develop drugs that would help reactivate the sensor and therefore activate apoptosis.”
One of those sensors is a well-studied protein called p53. When it functions normally, it suppresses the formation of cancer through apoptosis. Mutations in the p53 gene are found in about half of all cancers.
Other Forms of Cell Death
Another common form of cell death is necrosis, which occurs when a cell is injured or ruptured. “Historically we thought that necrosis just happened in response to an injury, for example a burn or a cut,” Dr. Overholtzer says. “In the past five years, however, studies have shown that necrosis is also programmed, but in a completely different way than apoptosis.”
A third well-studied type is called autophagy, in which a cell breaks down and digests itself. Autophagy can occur as a natural part of growth and development, but it can also be a response to certain diseases or stress, such as infection. Similar to apoptosis, autophagy can play a role in cancer, if it doesn’t occur when it should and cells are able to grow out of control.
Dr. Overholtzer’s lab is studying yet another kind of cell death, called entosis, in which one cell engulfs another and kills it. “Entosis is a completely different process,” he says. “The other types of cell death are all forms of suicide, but this is really a murdering event.”
He first discovered entosis as a postdoctoral fellow while studying breast cancer cells under a microscope, when he observed some of the cancer cells entombing neighboring cells. Some of the captured cells escaped unharmed, and some were able to continue dividing inside the host cell, but most eventually died.
Other cases of cells murdering cells that have been observed are different because they result from two different cell types, which are in many cases also distinct genetically, competing against each other. “In this case, cells are killing cells that are identical to themselves,” Dr. Overholtzer says. “We’ve even seen cases where a cell has divided and one daughter cell kills the other one.”
Investigators don’t know yet whether entosis occurs in healthy, normal cells, but it’s something that Dr. Overholtzer and his team are continuing to study.
“Any time you have a new window into how cell death works, particularly a program that you can see going on in a tumor, that’s a real opportunity to dive in and see if you can learn how to manipulate it with the goal of finding new cancer treatment strategies,” he concludes.
July 29, 2019, by NCI Staff
 Enlarge
Enlarge
A live cell (a) and cells undergoing apoptosis, where cells shrink as they die (b); necroptosis, where a cell swells before bursting (c); and necrosis, where a cell and its organelles are ruptured (d).
Credit: Sci Rep. 2016. doi: 10.1038/srep21992. CC BY 4.0.
New research suggests that inducing a form of controlled cell death called necroptosis in or around tumor cells can help the immune system rid the body of cancer cells.
Necroptosis is an explosive form of cell death during which a cell typically swells and then bursts. In the study, researchers found that injecting cells undergoing necroptosis into tumors in mice kickstarted an immune response against the tumors.
In the NCI-funded study, published June 21 in Science Immunology, the researchers also used a virus to deliver genes for the proteins that drive necroptosis into tumor cells. Combining this treatment with a commonly used form of immunotherapy proved to be highly effective at eliminating tumors in mice, they reported.
Andrew Oberst, Ph.D., an immunologist at the University of Washington, who led the project, sees these as pilot experiments. “The findings are promising in thinking about how necroptosis could be deployed in the clinic someday, after significant additional development.”
Testing Necroptosis in Mice
The body uses several different methods of cell death to rid itself of abnormal, harmful, or unneeded cells. Researchers believe necroptosis is the body’s method of killing cells infected by viruses, Dr. Oberst explained. Necroptotic cells flood the area around infected cells with small signaling molecules called cytokines that can trigger inflammation and attract immune cells.
“The kind of immune response that happens with viral infections is also the response cancer immunotherapy tries to trigger, so we hoped that necroptosis would stimulate some of those same pathways to help clear the body of cancer cells,” he added.
“Any cancer treatment is aimed at killing cancer cells, but how cells die is important,” explained Konstantin Salnikow, Ph.D., a program director in NCI’s Division of Cancer Biology. In order to eliminate cancer cells from the body more effectively, “we need to move toward cancer treatments that provoke an immune response,” Dr. Salnikow said.
To start, Dr. Oberst’s team had to see if inducing necroptosis would help the immune system fight cancer cells. They knew from past studies that to start necroptosis they had to activate the protein kinase RIPK3, which works with other proteins in the cell to start the process of self execution.
Annelise Snyder, Ph.D., then a graduate student in Dr. Oberst’s lab, activated RIPK3 protein in tumor cells to make them necroptotic. She then injected the engineered necroptotic cells into either melanoma or adenocarcinoma tumors implanted under the skin of mice. The necroptotic cells slowed down tumor growth and helped the mice live longer than when Dr. Snyder injected apoptotic cells into the tumors. Apoptosis is a tidier form of controlled cell death than necroptosis that does not release inflammatory signals into surrounding tissue.
Next, Dr. Snyder activated RIPK3 protein in normal rather than cancerous cells and found the same result: Injecting the necroptotic cells into tumors slowed their growth and helped the mice live longer.
The finding, Dr. Oberst said, showed that the dying cells were activating an immune response in the tumor that did not depend on the immune system recognizing specific markers on cancer cells.
“We initially thought that the response would depend on tumor cells needing to die, but the necroptotic cells are changing the tumor microenvironment to recruit immune cells in the area,” Dr. Oberst said.
Further tests showed that the inflammatory signals from necroptotic cells were necessary to slow tumor growth. Additionally, the necroptotic cells appear to recruit and activate phagocytes a type of immune cell that can engulf and ingest unwanted cells. When cancer cells were labeled with fluorescent protein before necroptotic cells were introduced, those fluorescent proteins ended up in phagocytes, showing that the activated immune system had absorbed tumor cells.
Stimulating the Immune System
Rather than injecting necroptotic cells into mouse tumors, the researchers found they could instead deliver an activated form of the RIPK3 gene into tumor cells using an engineered virus. The virus infected tumor cells and the activated RIPK3 triggered necroptosis, slowing tumor growth and improving how long the mice lived.
Dr. Oberst says he can see delivering RIPK3 into tumors as a therapeutic approach for humans in the future. Regardless of the delivery method—using a virus, RNA injection, or nanoparticles—generating an active form of the enzyme in tumors is likely to help suppress their growth, Dr. Oberst said.
Finally, the study showed that treating mice with an immune checkpoint inhibitor and inducing necroptosis in the tumor at the same time had a synergistic effect. That is, the combination killed cancer cells far more effectively than either treatment approach alone, fully eliminating tumors in most of the mice and preventing the same type of cancer cells from establishing a new tumor.
Next Steps
Douglas Green, Ph.D., an immunologist at St. Jude Children’s Research Hospital, who was not involved in the study, said that this approach of combining necroptosis with immunotherapy has promise. “This work is at the cutting edge of research on cell death and tumor immunotherapy.”
He added, “I hope that we will see a direct extension of this work into practical, effective cancer treatment. The strategy the authors outlined is readily adaptable for human use.”
Dr. Salnikow cautioned that it is difficult to predict how successfully and how soon this approach could be implemented. But, he said, this work provides an important advance in knowledge about anti-tumor immunity.
To help develop their findings for possible clinical application, Dr. Oberst and his team have begun working with industry partners. They are starting to extend their findings to different mouse models that better mimic human cancer.
Because cancer cells that arise in different tissues may produce different inflammatory signals when they undergo necroptosis, the researchers are also working to understand which cytokine signals released by necroptotic cells are most important in activating an immune response in different tumors. Understanding these differences, they believe, could help them engineer better approaches to drive an immune response in different types of cancers.